Blood fats play key role in peripheral neuropathy for patients with type 2 diabetes
XXIII WCN 2017, Kyoto, Japan, 16-21 September 2017
Kyoto (ptp008/21.09.2017/09:00) Controlling a young diabetic patient's blood sugar is not enough to ward off diabetic peripheral neuropathy, or nerve pain, according to a University of Michigan study that demonstrated the pronounced role of obesity-related metabolic syndrome in the development of the nerve disorder.
The study, Prevalence and Risk Factors for Diabetic Peripheral Neuropathy in Youth with Type 1 and Type 2 Diabetes: SEARCH for Diabetes in Youth Study, was presented by senior author Prof Eva L. Feldman, MD, PhD, at the World Congress of Neurology. This major scientific event takes place in Kyoto, Japan, from 16 to 21 September 2017. The study also appeared in the September 2017 issue of the journal Diabetes Care.
"Diabetes is reaching epidemic levels in western society, and correspondingly, debilitating complications such as peripheral neuropathy impact people at younger and younger ages," said Prof Feldman. "It is essential that we join forces at the international level and coordinate a concerted action plan to address these crucial problems. To this end we have recently, at the Peripheral Neve Society meeting in Sitges, formed an international working group for the promotion of research on and treatment of diabetic neuropathy on a global scale. I hope we can mobilize our partners from all regions of the world." This will also be an important topic at the International Congress for Neuromuscular Diseases ICNMD 2018 which will take place in Vienna, Austria, in July next year.
It has long been suspected that glycemic control, while being an important factor in diabetic peripheral neuropathy, is not the only one. "Metabolic syndrome, prompted by obesity and a driver of dyslipidemia, also has a considerable impact. In fact, our study showed that obesity alone can cause neuropathy," Prof Feldman said.
Researchers supported the finding with results of a clinical trial to reverse neuropathy in Type 2 diabetes, conducted by the University of Michigan and the University of Utah. In the clinical trial, patients with pre-diabetes or newly diagnosed Type 2 diabetes were prescribed 30 minutes a day of exercise and a goal of losing 7 percent of their body weight. Those who exercised and lost weight saw their neuropathy reversed. When exercise and dieting ceased, neuropathy returned.
Further, the University of Michigan study showed that diabetic peripheral neuropathy is more prevalent in young people with Type 2 diabetes: 22 percent for subjects with Type 2 diabetes and 7 percent for subjects with Type 1 diabetes.
The study was conducted using enrollees from the SEARCH for Diabetes in Youth study, which included 2,777 subjects from Ohio, Washington, South Carolina, Colorado, California, and Native American populations in Arizona and New Mexico. Of those, there were 1,734 youths with Type 1 diabetes and 258 with Type 2 diabetes who had complete data for variables of interest. The cohort of subjects was multiethnic.
The study found that glycemic control and diabetes duration were critical factors in the development of peripheral neuropathy. Prior studies have shown that good glycemic control could potentially delay peripheral neuropathy; this study confirmed that glycemic control over time was significantly worse in subjects with diabetic peripheral neuropathy than in those without.
Additionally, subjects with Type 2 diabetes for more than 10 years showed a 36 percent prevalence of diabetic peripheral neuropathy, compared with 19 percent for those who had Type 2 diabetes for 5-10 years. Similarly, subjects with Type 1 diabetes for more than 10 years showed a 13 percent prevalence compared to 5 percent for those with Type 1 diabetes for 5-10 years.
Source: Prevalence of and Risk Factors for Diabetic Peripheral Neuropathy in Youth With Type 1 and Type 2 Diabetes: SEARCH for Diabetes in Youth Study: Mamta Jaiswal, Jasmin Divers, Dana Dabelea, Scott Isom, Ronny A. Bell, Catherine L. Martin, David J. Pettitt, Sharon Saydah, Catherine Pihoker, Debra A. Standiford, Lawrence M. Dolan, Santica Marcovina, Barbara Linder, Angela D. Liese, Rodica Pop-Busui and Eva L. Feldman. Diabetes Care 2017 Sep; 40 (9): 1226-1232
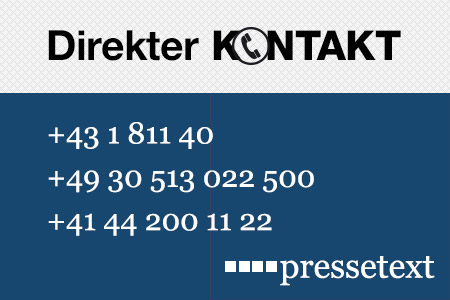
Contact University of Michigan: Dave Spratt, T +1 (734) 998-1214, dspratt@umich.edu
(end)| Aussender: | Bettschart & Kofler Kommunikationsberatung GmbH |
| Ansprechpartner: | Dr. Birgit Kofler |
| Tel.: | +49-30-700 159 676 |
| E-Mail: | kofler@bkkommunikation.com |
| Website: | www.wfneurology.org |